If you’ve ever felt a burning sensation in your chest after a meal and thought “heartburn” you’re not alone. Gastroesophageal reflux disease (GERD) is one of the most common digestive concerns for many adults.
In simple terms, GERD happens when stomach acid flows backward into the esophagus (the swallowing tube), causing irritation and that familiar burning or sour taste in the back of your throat. Over time, repeated acid exposure can inflame the lining of the esophagus and may lead to complications if not treated.
This article will walk you through who is more likely to develop GERD, how we diagnose and treat it, some natural and lifestyle strategies that help, and when your heartburn could be something other than GERD.
Important note: This article is for education purposes and is not a substitute for seeing your own doctor. If you ever have severe chest pain, trouble breathing, or pain going into your arm or jaw, call 911 or go to the ER immediately.
How Common Is GERD: Who Is a Higher Risk?
Worldwide, about 1 in 7 people have GERD, with rates in North America closer to 1 in 5 adults. Certain factors make GERD more likely:
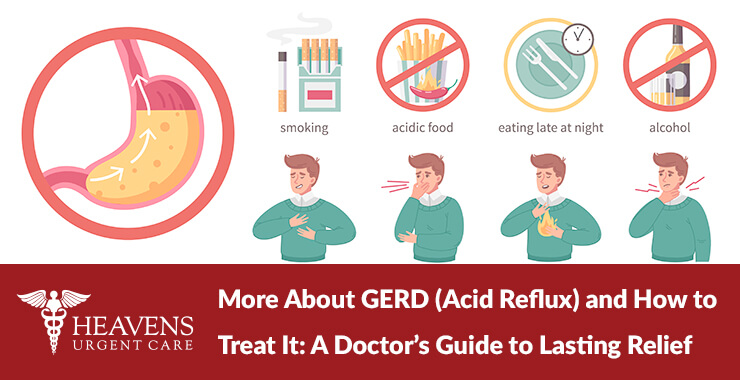
- Excess weight or obesity – Extra abdominal pressure can push stomach contents up into the esophagus.
- Older age – The risk increases as we get older, partly due to changes in muscles and tissues that keep stomach acid where it belongs.
- Hiatal hernia – When part of the stomach slides up into the chest, it can weaken the valve between the esophagus and stomach.
- Pregnancy – Hormonal changes and pressure from the growing uterus often worsen reflux.
- Certain foods and drinks – Coffee, chocolate, spicy or fatty foods, citrus, carbonated drinks, and alcohol can trigger or worsen symptoms for some people.
- Smoking and vaping – Nicotine relaxes the valve (lower esophageal sphincter) that normally keeps acid down.
- Medications – NSAIDs (like ibuprofen), some blood pressure medicines, and others can irritate the esophagus or worsen reflux.
- Family history and stress – Having relatives with reflux and high stress levels have both been linked to higher GERD risk.
You don’t have to tick every box on this list to have GERD, but the more factors you have, the more it’s worth having a conversation with your doctor.

Typical GERD Symptoms: Plus, a Few Surprises
Common GERD symptoms are burning in the chest (heartburn), often after eating or when lying down. A sour, bitter, or acidic taste in the mouth and regurgitation (food or liquid coming back up). Some people report a feeling of “something stuck” in the throat, hoarseness, chronic throat clearing, or a chronic cough.
Others say that they have worse symptoms at night or when they lie flat. While others hardly ever feel heartburn but have cough, hoarseness, or asthma-like symptoms, especially at night. This is sometimes called “extra-esophageal reflux” and can be trickier to recognize.
How We Diagnose GERD
Most of the time, GERD is diagnosed clinically based on your symptoms, history, and risk factors. If your symptoms are classic and uncomplicated, your medical provider will often start with lifestyle changes and a short trial of medication to see if you improve.
Depending on your situation, your doctor might also consider these three options.
- Upper endoscopy (EGD): A small camera looks at the esophagus and stomach to check for inflammation, ulcers, strictures (narrowing), or precancerous changes.
- pH monitoring: A small probe measures how often and how long acid is coming up into the esophagus.
- Esophageal manometry: Measures how well your esophagus muscles and valve are working.
In my Tempe, Arizona practice, I especially likely to order tests if my patients:
- have difficulty swallowing, food getting stuck, or pain when swallowing
- have had symptoms for many years
- are over 50 with new or worsening symptoms
- have unintentional weight loss, vomiting, anemia, or blood in stool
These types of red flags are signs that tell me that I need a closer look.
GERD Treatment: What Actually Works
Lifestyle Changes
You’ll often hear a long list of “don’ts” for GERD. The science is actually a bit more nuanced. Large reviews of lifestyle changes have found strong evidence for a few key strategies:
- Weight loss (if overweight): Even a modest reduction in weight can significantly reduce reflux episodes.
- Elevate the head of the bed: Raising the head of your bed by 6–8 inches (using blocks or a wedge pillow) helps gravity keep acid down at night.
- Avoid lying down within 3 hours of a meal: Late-night dinners plus bedtime is a common reflux trap.
- Smaller, more frequent meals: Big meals increase pressure in the stomach and make reflux more likely.
Helpful, but more individualized lifestyle changes include:
- Identifying your trigger foods (spicy, fatty, fried, tomato-based, citrus, chocolate, peppermint, carbonated drinks, alcohol).
- Cutting back on alcohol and smoking or vaping.
- Managing stress through practices like gentle exercise, breathing exercises, meditation, or counseling as stress can amplify how we feel symptoms, even if it doesn’t cause GERD by itself.
I tell my patients that medication can help, but lifestyle is what gives us long-term traction.
Medications
Medications for GERD fall into a few categories.
- Antacids (Tums®, Maalox®, etc.): These work quickly to neutralize acid and are good for occasional symptoms but not a long-term fix.
- H2 blockers (famotidine/Pepcid®, etc.): Blockers reduce acid production for several hours. They are helpful for mild to moderate symptoms or as a step-down option from stronger meds.
- Proton pump inhibitors (PPIs) (omeprazole, pantoprazole, esomeprazole, etc.): These are the most powerful acid-suppressing drugs and are often first-line for moderate to severe GERD or esophagitis. Guidelines recommend taking PPIs 30–60 minutes before a meal for best effect.
PPIs are effective and generally safe, but like any long-term medication, they need to be used thoughtfully. We want to weigh the benefits versus the potential risks (like nutrient malabsorption, infections, or bone density concerns) and periodically reassess whether you still need them at the same dose.

When Is Surgery or a Procedure Considered?
If lifestyle changes and medications don’t control symptoms, or if you can’t tolerate medications, a gastroenterologist might discuss either a laparoscopic fundoplication (wrapping part of the stomach around the lower esophagus to strengthen the valve and prevent reflux.) or a magnetic sphincter augmentation (LINX device) which is a ring of magnetic beads around the lower esophagus that opens for swallowing and closes to prevent reflux.
These options are typically reserved for carefully selected patients after thorough evaluation.
Natural and Complementary Approaches to GERD
Many patients ask, “Are there natural ways to manage GERD beyond just avoiding certain foods?”
Here’s what current research suggests:
- Alginates – Alginates are compounds derived from brown seaweed. They form a “raft” that floats on top of stomach contents and helps block acid from refluxing into the esophagus. Studies show alginate-based formulations can improve GERD symptoms and are often used alongside or instead of traditional antacids. These are available over the counter, but it’s still wise to ask your doctor if they’re appropriate for you, especially if you’re on other medications.
- Herbal and Nutritional Support – A 2025 review of natural products for GERD found promising, but early, evidence for ginger, licorice (DGL), probiotics, slippery elm, Aloe vera, and melatonin, among others. These may help protect the esophageal lining, lessen inflammation, or support motility.
Key things to remember when considering herbal and nutritional support:
- Many studies are small or short-term.
- Herbal products can interact with medications (for example, licorice and blood pressure or potassium levels).
- Natural doesn’t always mean safe for everyone.
If you’re interested in these approaches, I’m very open to integrating them, but I want to do it safely, with your full medical picture in mind.
- Mind–Body and Lifestyle Habits – GERD lives at the intersection of biology and lifestyle. While acid and anatomy are the primary drivers, stress and sleep also matter. Helpful habits include gentle, regular movement, like walking, to support digestion and weight management. I also recommend stress reduction through breathing exercises, yoga, or mindfulness, and improving sleep posture (head-up position, left-side sleeping) to reduce nighttime reflux.
Could It Be Something Other Than GERD?

This is one of the most important questions I want my patients to ask. That’s because many conditions can mimic GERD or coexist with it, including:
- Heart disease (angina or heart attack)
- Chest pressure or pain that may radiate to the arm, neck, jaw, or back
- Shortness of breath, sweating, nausea, or feeling faint. This is a medical emergency. If you’re unsure whether it’s heartburn or your heart, seek emergency care.
- Peptic ulcer disease
- Burning or gnawing pain, often between meals or at night
- Sometimes associated with Helicobacter pylori (H.pylori) infection or long-term NSAID use
- Gallbladder disease (biliary colic)
- Right upper abdominal pain after fatty meals
- Pain can radiate to the back or right shoulder
- Eosinophilic esophagitis or inflammation in the esophagus related to allergies
- Trouble swallowing, food getting stuck, or chest discomfort
- Esophageal motility disorders (such as achalasia or esophageal spasm)
- Chest pain and swallowing problems that don’t respond to typical GERD treatment
- Functional heartburn or hypersensitive esophagus
- Symptoms of heartburn but no clear acid reflux on testing
- Often related to nerve sensitivity and sometimes stress or anxiety
Avoid self-diagnosing chronic heartburn because it can be risky. If your symptoms are new, worsening, not improving on medication, or accompanied by red flags like trouble swallowing, weight loss, blood in vomit or stool, anemia, please see your doctor right away.
GERD FAQ: Questions I Hear Most Often
Q: Can GERD cause a cough or throat problems?
A: Yes. GERD doesn’t always show up as classic heartburn. For some people, acid and non-acid reflux can irritate the throat and voice box and lead to chronic cough, frequent throat clearing, hoarseness, or voice changes. Some patients report the sensation of a lump in the throat. We sometimes call this laryngopharyngeal reflux (LPR) or silent reflux because patients may not feel much burning in the chest. If you’ve had a chronic cough or voice issues that haven’t resolved with allergy or asthma treatment, it’s worth talking to your doctor about possible reflux.
Q: Is long-term PPI use safe?
A: Proton pump inhibitors (PPIs) are very effective at reducing acid and healing inflammation in the esophagus. For many people, a limited course (usually 4–8 weeks) is enough to bring symptoms under control, after which we can often step down to a lower dose, an H2 blocker, or lifestyle management alone.
For some patients, especially those with severe esophagitis, Barrett’s esophagus, or certain complications, long-term PPIs are appropriate and protective. That said, long-term use has been associated in some studies with possible risks like nutrient malabsorption (B12, magnesium), bone density changes, and certain infections.
My approach is to use the lowest effective dose for the shortest necessary time. Reassess periodically whether you still need the medication, and to support overall health with good nutrition, movement, and monitoring when appropriate.
If you’re on a PPI and worried about long-term effects, don’t stop suddenly taking the medication. Let’s talk first and make a step-down plan together if it’s safe to do so.

Q: Are there specific foods I should always avoid if I have GERD?
A: There’s no one GERD diet that works for everyone, but some foods are more likely to trigger symptoms. They are:
- High-fat or fried foods
- Spicy foods
- Tomato-based sauces
- Citrus fruits and juices
- Chocolate or peppermint
- Carbonated drinks and alcohol
- Large, heavy meals
Rather than cutting everything forever, I usually recommend starting with a short trial elimination diet of the most common triggers. Additionally, I ask my patients to keep a simple food–symptom diary for 1–2 weeks, then we reintroduce foods one at a time so they can see which ones are truly a problem. The goal isn’t a miserable, ultra-restricted diet it’s to learn your body’s patterns so you can enjoy food with less discomfort.
Q: Can GERD go away on its own?
A: Occasional heartburn after a heavy meal may come and go. But chronic GERD includes symptoms that occur more than twice a week, or symptoms that have been around for months or years usually doesn’t fully abate without some combination of:
- Lifestyle changes
- Weight loss if appropriate
- Medication
- Or, in select cases, a procedure
The good news is that many patients see a big improvement with relatively small adjustments (like meal timing, bed elevation, and a short course of medication). The earlier we address GERD, the easier it is to prevent long-term complications.
Q: Is GERD dangerous?
A: GERD is common and very treatable, but uncontrolled, long-standing reflux can lead to complications such as:
- Esophagitis (inflammation)
- Narrowing (strictures) that make swallowing difficult
- Barrett’s esophagus (changes in the cells lining the esophagus)
- A small increased risk of esophageal cancer in some patients with Barrett’s
This is why I take persistent reflux seriously. Our goal isn’t just to relieve discomfort, it’s also to protect the esophagus over the long term.
Q: How do I know if my “heartburn” is actually my heart?
A: Thank you for asking this vital question. Heartburn and heart-related chest pain can feel similar. You should seek emergency care (call 911) if you have:
- Chest pressure, squeezing, or pain that lasts more than a few minutes
- Pain that radiates to your arm, neck, jaw, or back
- Shortness of breath, sweating, nausea, or feeling faint
If you’re not sure whether it’s your heart or GERD, treat it as an emergency. I would much rather you be evaluated and reassured than ignore a serious problem.
Q: What’s one simple change I can make today to help my GERD?
A: If I had to choose just one small change with a big impact, it would be this: Avoid lying down within 3 hours of eating and elevate the head of your bed. For many patients, simply changing evening routines like earlier, lighter dinners and a slightly elevated sleeping position reduces nighttime reflux, improves sleep, and lessens the need for rescue medications.
When Should I See a Doctor or Go to Urgent Care?
You should schedule an appointment with a primary care physician or gastroenterologist if:
- You have heartburn or reflux symptoms more than twice a week
- Over-the-counter medications only help temporarily, or not at all
- You’ve used antacids or acid-suppressing meds regularly for weeks without medical guidance
- You have long-standing GERD and want to discuss long-term risks and prevention
You should seek urgent or emergency care if:
- You have chest pain with shortness of breath, sweating, nausea, or pain radiating to the arm, neck, jaw, or back
- You’re vomiting blood or material that looks like coffee grounds
- Your stools are black and tarry
- You suddenly can’t swallow or feel as if food is stuck in your throat
If you’re dealing with GERD symptoms, you’re not being dramatic or picky. You are simply listening to your body, and that’s a good thing. I want you to feel encouraged because GERD is very treatable. With the right combination of lifestyle changes, the thoughtful use of medications, potentially adding natural options and, when needed, further testing you can get back to eating, sleeping, and living with far less discomfort.
If you’re not sure whether what you’re feeling is GERD, or you’re worried it might be something more serious, please reach out to me at (623) 444-2734.